Is The Danger of NTG in RVMI a Medical Myth?
It's common to find RVMI a contraindication or caution to NTG administration. Is this actually supported by the evidence?
Current Practice
Sublingual (SL) low dose nitroglycerin (NTG) 0.3 – 0.4mg q 5min x3 is the front line treatment for chest pain of suspected Acute Coronary Syndrome (ACS) origin in the prehospital and emergency environments[1,5,6]. While evidence supporting the outcome benefit of SL NTG in ACS is lacking[2], its effectiveness in reducing ACS symptoms is not[3,4].
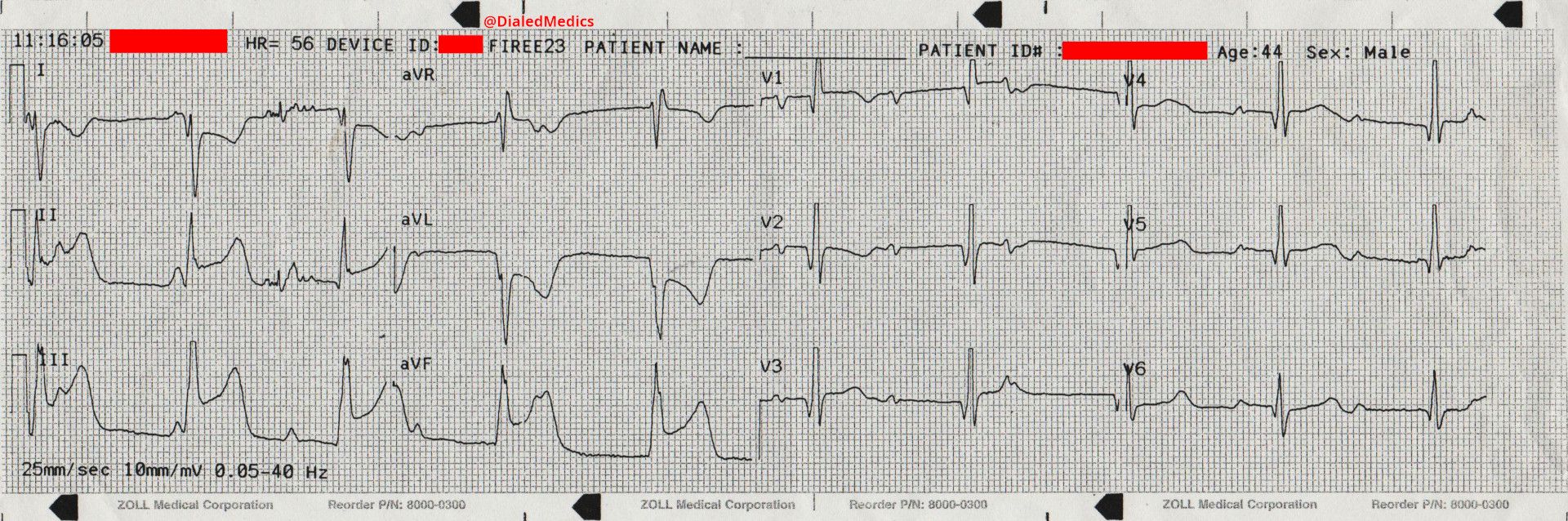
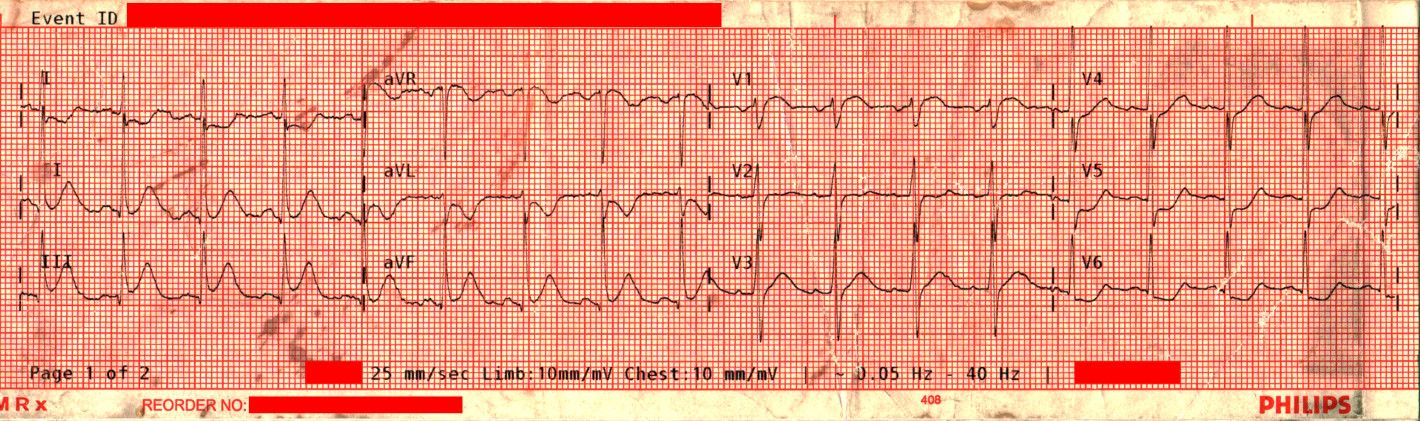
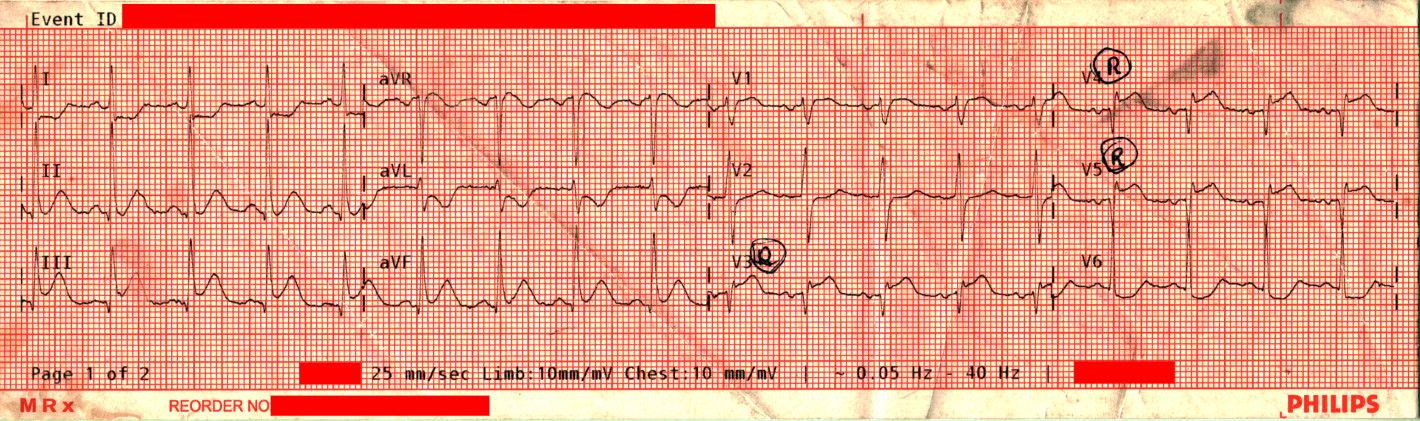
Most protocols caution or contraindicate SL NTG use in the presence of Right Ventricular Myocardial Infarction (RVMI)[5,6]. The 2015[20] and 2020[7] American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care do not update the still standing 2010[6] recommendation addressing NTG in RVMI, which states:
Administer nitrates with extreme caution, if at all, to patients with inferior STEMI [ST Elevation Myocardial Infarction] and suspected right ventricular (RV) involvement because these patients require adequate RV preload.
The guidelines are unclear about which patients do not require adequate RV preload and this recommendation is not referenced in either of the cited sources. Although the important role that preload plays during RVMI is well established[8], its relationship to low dose SL NTG seems poorly understood based on the discussions presented here[9,11]. This leaves two important questions for clinicians treating emergent ACS symptoms:
- Does SL NTG precipitate a decrease in Blood Pressure (BP) during RVMI moreso than other locations of Obstructive Myocardial Infarction (OMI)?
And, as we know that SL NTG is associated with transient episodes of hypotension[5,18]:
- In the unavoidable cases where SL NTG does induce hypotension, are RVMI patients at greater risk for adverse events (AE) or worse outcomes?
The History of the Current Practice
In 2016 Air Medical Journal published Inferior Wall Acute Myocardial Infarction: Not as Preload Dependent as Once Thought?[9] A literature review on this topic finding:
Retrospective cohort studies from the 1980's and 1970's first documented the prevalence of profound hypotension in patients with IWMI [Inferior Wall Myocardial Infarction] and RVMI after the administration of NTG.
Of the largest and most prominent of those studies (Ferguson et al., 1989[10]) the review found:
Despite the limitations of a small sample size and simultaneous administration of a calcium channel blocker in a number of patients, and conceding that right-sided 12-lead ECGs were not 100% specific or sensitive to RVMI, Ferguson et al. concluded there was a strong association of nitrate-dependent hypotension in IWMI. The study also did not report the rates of hypotension in isolated IWMI or RVMI.
The Australasian Journal of Paramedicine in 2021 published Right Ventricular Myocardial Infarction and Adverse Events From Nitrates: A Narrative Review[11]. Taking note of the 1989 research by Ferguson et al.[10] it reported:
The view against the use of nitrates during RVMI can be traced back to a single 1989 cohort study of 28 patients, then later being adopted by a series of influential secondary evidence papers, and ultimately by international guidelines.
Together, these two reviews record a detailed history of the caution recommendation for SL NTG in RVMI and find that evidence is lacking[9,11]. If this is the case, what evidence exists to guide emergent ACS treatment with SL NTG?
Evidence for the Safety of NTG in RVMI
Wilkinson goes on to look at some recent research, reviewing three studies[11]:
- Prehospital Nitroglycerin Safety in Inferior ST Elevation Myocardial Infarction[12] (2016) - Prehosp Emerg Care | Conclusion:
Our study suggests that nitroglycerin administration to patients with chest pain and inferior STEMI on their computer-interpreted ECG is not associated with a higher rate of hypotension compared to patients with STEMI in other territories. Computer-interpreted prehospital ECGs indicating an inferior STEMI cannot be used as the sole predictor for patients who may be at higher risk for hypotension following NTG administration. (emphasis added)
- Prehospital Adverse Events Associated With [NTG] Use in STEMI Patients With Right Ventricle Infarction[13] (2017) - Canadian Journal of Emergency Medicine | Conclusion:
Results of this study suggest no difference in the rate of AEs between patients with inferior STEMI and STEMI with RVI when NTG is administered in the prehospital setting. (emphasis added)
- Safety and Effectiveness of Field Nitroglycerin in Patients with Suspected ST Elevation Myocardial Infarction[14] (2019) - Prehosp Emerg Care | Conclusion:
In this cohort of suspected or confirmed STEMI patients, field NTG resulted in pain reduction and did not result in a clinically significant decrease in blood pressure when compared with patients who did not receive NTG, nor an increased frequency of hypotension or bradycardia on ED arrival. (emphasis added)
After review Wilkinson concludes that:
Of the cohort studies of primary evidence, the three chohort studies published from 2016 to present, cumulatively including 1046 patients, found nitrates could be administered without increased risk, while the 1989 cohort study of 28 patients remains the only cohort evidence suggesting increased risk. (emphasis added)
Most recently (2022) the British Medical Journal published Adverse Events From Nitrate Administration During [RVMI][15] reporting:
Meta-analysis was possible for sublingual nitroglycerin 400 mcg (2 studies, n=1050) and found no statistically significant difference in relative risk to combined inferior and RVMI at 1.31 (95% CI 0.81–2.12, p=0.27), with an absolute effect of 2 additional adverse events per 100 treatments. (emphasis added)
And after a discussion of limitations concluded:
This review suggests that the contraindication on nitrate administration during RVMI is not supported by the evidence in forming this appraisal for 400mcg sublingual nitroglycerin. (emphasis added)
It is reported that 40% of Myocardial Infarctions (MI) involve the inferior wall[16] with 40-50% of those being RVMI[8]. With that in mind, there is good evidence for the safety of NTG in region unspecific OMI. In 1994 Annals of Emergency Medicine published Safety of Prehospital Nitroglycerin[21] noting:
Our findings are consistent with previous reports in that the adverse reactions to [NTG] appeared idiosyncratic. It is well known that patients with an [IWMI] or [RVMI] are prone to develop hypotension when given [NTG], primarily because of reduced left ventricular filling pressures. However, in approximately 50% of previous reports of this syndrome, there was no evidence of an acute [MI], and this was also the percentage of our adverse effect patients who has a final diagnosis of acute [MI]. (emphasis added)
And concluded with:
[SL NTG] is a well-known and relatively safe prehospital drug: however, ALS [Advanced Life Support] providers and medical control physicians should be aware of potentially serious adverse reactions. Based on our data these may occur in 1.3% of treated patients... ...Pretreatment characteristics of our patients appeared to be of no help in predicting these reactions. (emphasis added)
A year before that in 1993 Prehospital Disaster Medicine published The Prehospital Use of Nitroglycerin According to Standing Medical Orders in an Urban EMS System[22], finding:
Nitroglycerin is under-utilized in this prehospital setting. The administration of sublingual NTG is safe and effective in prehospital care of patients assessed with ischemic chest pain or pulmonary edema. There is no justification for withholding NTG re-administration according to protocol as long as no significant adverse reactions have occurred. Further, it appears that NTG should not be withheld in patients lacking intravenous access. Fear of serious adverse reactions seemingly are unfounded as they appear to be rare and limited. (emphasis added)
A 2000 publication in Prehospital Emergency Care, Effects of Prehospital Nitroglycerin on Hemodynamics and Chest Pain Intensity[17] found:
The results of our study indicate that administration of [SL] NTG to patients presenting with CP of suspected cardiac origin or CHF in the prehospital setting is safe. Although rapid establishment of IV access is recommended in all patients with suspected chest pain of ischemic origin or CHF, we do not feel that withholding sublingual NTG in patients without IV access is justified. (emphasis added)
Although the findings of this study did not report on RVMI they also mention the possible risk associated with NTG citing Ferguson et al.[10] once again. Prehospital Emergency Care also published Prehopsital Nitroglycerin in Tachycardic Chest Pain Patients: A Risk for Hypotension or Not?[19] in 2016 where it was reported:
...we still cannot predict reliably which patients will develop adverse effects [to SL NTG]. In the literature, a minority of adverse effects in prehospital patients were serious. ...Our findings suggest that there is an association between tachycardia and hypotension in patients administered NTG for chest pain, with tachycardic patients showing rates of hypotension 33% higher than non-tachycardic patients. However, the results showed an absolute difference in risk of only 1%. (emphasis added)
Concluding with:
The results of this study indicate that there was a statistically significant increase in the relative risk of hypotension with NTG administration in tachycardic patients. However, the absolute risk of NTG-induced hypotension was low in these patients. (emphasis added)
More recently in 2021 the American Journal of Emergency Medicine published Adverse Events After Prehospital Nitroglycerin Administration in a Nationwide Registry Analysis[17] identifying 80,760 NTG administration cases over 1,322 EMS agencies with an adverse event rate of 7% and came to the conclusion:
This large national prehospital study demonstrated that adverse events following NTG administration were more common than previously thought but rare in patients with an SBP > 110 and a HR < 100.
It would seem there is a preponderance of evidence that SL NTG is safe and effective in symptom management for chest discomfort of suspected ACS origin, both in OMI in general and in RVMI specifically.
So What?
SL NTG is generally given in the first 15 min. of contact with healthcare providers[23]. After which, the protocol has been exhausted (0.3 – 0.4mg q 5min x3) or symptoms have abated[5,6]. The current cautions and contraindications to SL NTG in suspected RVMI complicate this early and important phase of patient care, with one study included here reporting[13]:
Paramedics in our region do not preform 15-Lead ECGs. As a result patients experiencing a Right Ventricular Infarct (RVI) may receive [NTG]. In many cases, paramedics do not administer NTG to those with inferior STEMI out of concern that there may be an associated RVI. (emphasis added)
As The OMI Manifesto argued[24]:
Deciding which patients need emergent reperfusion therapy is complex, and our current criteria for doing so are not adequate to the task. The patients who benefit from emergent catheterization are those with acute coronary occlusion (ACO) or near occlusion, with insufficient collateral circulation, whose myocardium is at imminent risk of irreversible infarction without immediate reperfusion therapy.
Front loading symptom management (SL NTG) in ACS with a caution of dangerous hypotension based on the specific localization of infarct is a needless complication that is not supported in data and contradicted by the available evidence. Evidence is strong enough to contradict these cautions that SL NTG is recommended safe without IV access in several of the studies linked here[17,22] and is routinely used by patients themselves as well as BLS providers without access to EKG monitoring[7].
The goal of this post was not to look in detail at the quality of evidence available, most of the studies cited have discussions of their strengths and weaknesses included in them and several are literature reviews themselves. Instead the goal was to highlight the contrast in evidence for/against cautions and contraindications in SL NTG during suspected RVMI/IWMI.
That being said, a reveiw of the available information certainly seems to support the statement that the risk of SL NTG induced hypotension in suspected RVMI is a medical myth.
- Ferreira, Julio C B, and Daria Mochly-Rosen. Nitroglycerin use in myocardial infarction patients. Circulation journal: official journal of the Japanese Circulation Society vol. 76,1 (2012): 15-21. doi:10.1253/circj.cj-11-1133. Available at: ncbi.nlm.nih.gov | archive.org
- Salim Rezaie, The Death of MONA in ACS: Part III – Nitroglycerin, REBEL EM blog, November 5, 2017. Available at: rebelem.com | archive.org
- Boden, William E et al. Role of short-acting nitroglycerin in the management of ischemic heart disease. Drug design, development and therapy vol. 9 4793-805. 19 Aug. 2015, doi:10.2147/DDDT.S79116. Available at: ncbi.nlm.nih.gov | archive.org
- Engelberg S, Singer AJ, Moldashel J, Sciammarella J, Thode HC, Henry M. Effects of prehospital nitroglycerin on hemodynamics and chest pain intensity. Prehosp Emerg Care. 2000 Oct-Dec;4(4):290-3. doi: 10.1080/10903120090940967. PMID: 11045405. Available at: ncbi.nlm.nih.gov | archive.org
- Kim KH, Kerndt CC, Adnan G, et al. Nitroglycerin. [Updated 2021 Nov 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available at: ncbi.nlm.nih.gov | archive.org
- O'Connor RE, Brady W, Brooks SC, Diercks D, Egan J, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010 Nov 2;122(18 Suppl 3):S787-817. doi: 10.1161/CIRCULATIONAHA.110.971028. Available at: ahajournals.org | archive.org
- Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, Kudenchuk PJ, Kurz MC, Lavonas EJ, Morley PT, O’Neil BJ, Peberdy MA, Rittenberger JC, Rodriguez AJ, Sawyer KN, Berg KM; on behalf of the Adult Basic and Advanced Life Support Writing Group. Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(suppl 2):S366–S468. doi: 10.1161/CIR.0000000000000916. Available at: cpr.heart.org | archive.org
- Albulushi A, Giannopoulos A, Kafkas N, Dragasis S, Pavlides G, Chatzizisis YS. Acute right ventricular myocardial infarction. Expert Rev Cardiovasc Ther. 2018 Jul;16(7):455-464. doi: 10.1080/14779072.2018.1489234. Epub 2018 Jun 27. PMID: 29902098. Available at: ncbi.nlm.nih.gov | archive.org
- Jaton E. Inferior Wall Acute Myocardial Infarction: Not as Preload Dependent as Once Thought? Air Med J. 2017 Jan-Feb;36(1):27-29. doi: 10.1016/j.amj.2016.10.008. Epub 2017 Jan 4. PMID: 28089058. Available at: airmedicaljournal.com | archive.org
- Ferguson JJ, Diver DJ, Boldt M, Pasternak RC. Significance of nitroglycerin-induced hypotension with inferior wall acute myocardial infarction. Am J Cardiol. 1989 Aug 1;64(5):311-4. doi: 10.1016/0002-9149(89)90525-0. PMID: 2502902. Available at: ncbi.nlm.nih.gov | archive.org
- Wilkinson-Stokes M. Right ventricular myocardial infarction and adverse events from nitrates: A narrative review. Australasian Journal of Paramedicine [Internet]. 2021Mar.8 [cited 2022Jun.19];18. Available at: ajp.paramedics.org | archive.org
- Robichaud L, Ross D, Proulx MH, Légaré S, Vacon C, Xue X, Segal E. Prehospital Nitroglycerin Safety in Inferior ST Elevation Myocardial Infarction. Prehosp Emerg Care. 2016;20(1):76-81. doi: 10.3109/10903127.2015.1037480. Epub 2015 May 29. PMID: 26024432. Available at: ncbi.nlm.nih.gov | archive.org
- McConnell, A., Davis, M., Van Aarsen, K., Columbus, M., & Lewell, M. (2017). LO33: Prehospital adverse events associated with nitroglycerin use in STEMI patients with right ventricle infarction. CJEM,19(S1), S39-S39. doi:10.1017/cem.2017.95. Available at: www.lhsc.on.ca (PDF) | archive.org
- Bosson N, Isakson B, Morgan JA, Kaji AH, Uner A, Hurley K, Henry TD, Niemann JT. Safety and Effectiveness of Field Nitroglycerin in Patients with Suspected ST Elevation Myocardial Infarction. Prehosp Emerg Care. 2019 Sep-Oct;23(5):603-611. doi: 10.1080/10903127.2018.1558318. Epub 2019 Jan 28. PMID: 30556765. Available at: ncbi.nlm.nih.gov | archive.org
- Wilkinson-Stokes M, Betson J, Sawyer S Adverse events from nitrate administration during right ventricular myocardial infarction: a systematic review and meta-analysis BMJ Open 2022;12:doi: 10.1136/bmjopen-2022-EMS.1. Available at: bmjopen.bmj.com | archive.org
- Warner MJ, Tivakaran VS. Inferior Myocardial Infarction. [Updated 2022 May 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470572/. Available at: ncbi.nlm.nih.gov | archive.org
- Engelberg S, Singer AJ, Moldashel J, Sciammarella J, Thode HC, Henry M. Effects of prehospital nitroglycerin on hemodynamics and chest pain intensity. Prehosp Emerg Care. 2000 Oct-Dec;4(4):290-3. doi: 10.1080/10903120090940967. PMID: 11045405. Available at: ncbi.nlm.nih.gov | archive.org
- Popp LM, Lowell LM, Ashburn NP, Stopyra JP. Adverse events after prehospital nitroglycerin administration in a nationwide registry analysis. Am J Emerg Med. 2021 Dec;50:196-201. doi: 10.1016/j.ajem.2021.08.006. Epub 2021 Aug 8. PMID: 34390902; PMCID: PMC9029256. Available at: ncbi.nlm.nih.gov | archive.org
- Proulx MH, de Montigny L, Ross D, Vacon C, Juste LE, Segal E. Prehospital Nitroglycerin in Tachycardic Chest Pain Patients: A Risk for Hypotension or Not? Prehosp Emerg Care. 2017 Jan-Feb;21(1):68-73. doi: 10.1080/10903127.2016.1194929. Epub 2016 Sep 30. PMID: 27690207. Available at: ncbi.nlm.nih.gov | archive.org
- O'Connor RE, Al Ali AS, Brady WJ, Ghaemmaghami CA, Menon V, Welsford M, Shuster M. Part 9: Acute Coronary Syndromes: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015 Nov 3;132(18 Suppl 2):S483-500. doi: 10.1161/CIR.0000000000000263. PMID: 26472997. Available at: ncbi.nlm.nih.gov | archive.org
- Wuerz R, Swope G, Meador S, Holliman CJ, Roth GS. Safety of prehospital nitroglycerin. Ann Emerg Med. 1994 Jan;23(1):31-6. doi: 10.1016/s0196-0644(94)70004-4. PMID: 8273955. Available at: ncbi.nlm.nih.gov | archive.org
- Herman LL, Koenigsberg M, Ward S, Sloan EP. The prehospital use of nitroglycerin according to standing medical orders in an urban EMS system. Prehosp Disaster Med. 1993 Jan-Mar;8(1):29-33; discussion 34. doi: 10.1017/s1049023x00039972. PMID: 10155451. Available at: ncbi.nlm.nih.gov | archive.org
- Todoroski, K.B. The timing of administering aspirin and nitroglycerin in patients with STEMI ECG changes alter patient outcome. BMC Emerg Med 21, 137 (2021). https://doi.org/10.1186/s12873-021-00523-2. Available at: ncbi.nlm.nih.gov | archive.org
- Meyers HP, Weingart SD, Smith SW. The OMI Manifesto. Dr. Smith’s ECG Blog 2018. Available at: hqmeded-ecg.blogspot.com | drive.google.com
